BIOE Students Showcase Award-Winning Innovation at Capstone Expo
May 31, 2024
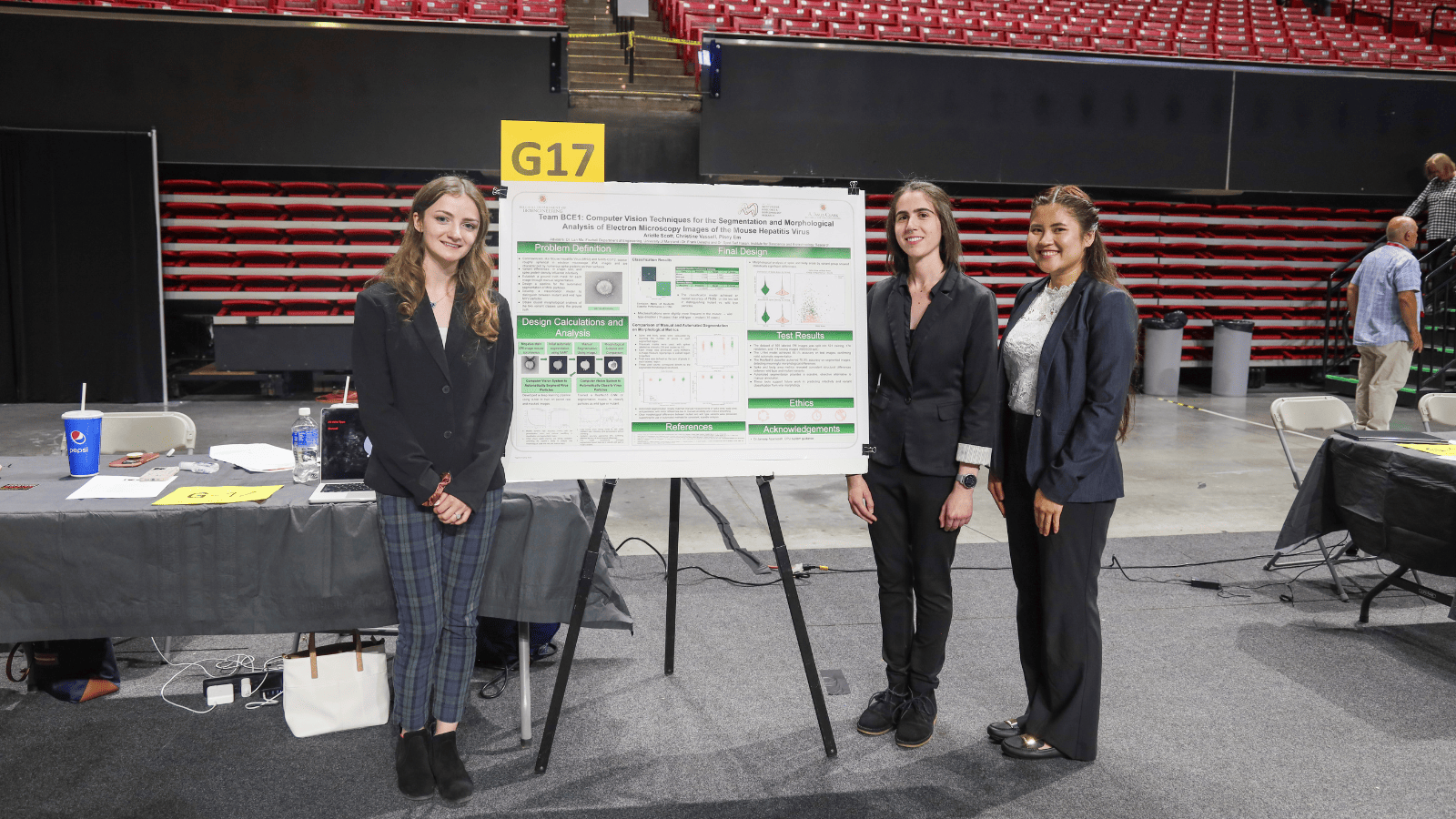
On May 1, the A. James Clark School of Engineering hosted its first annual Capstone Design Expo, showcasing the ingenuity and hard work of over 500 engineering seniors from the civil and environmental, aerospace, mechanical, and bioengineering programs. Held at the University of Maryland’s Xfinity Center, the Expo featured 98 projects offering solutions to some of society’s most pressing challenges. Students from the Fischell Department of Bioengineering’s (BIOE) bioengineering and biocomputational engineering undergraduate programs presented 20 projects focused on advancing healthcare and technology for medical diagnostics.
Six bioengineering teams received awards at the Expo, including the first-ever Dean’s Award for best overall capstone project. The Dean’s Award and its $1,000 cash prize were awarded to BIOE Team 9 for their design “Accessible Ventilation Coach for Opioid Overdose Bystanders,” a device that empowers bystanders and non-EMTs to properly and safely provide overdose victims with rescue breaths.
BIOE departmental awards included 1st place, 2nd place, and 3rd place awards, the Award for Translation Design Award, and the MPower Award.
The Award for Translational Design is sponsored by the Fischell Department of Bioengineering Advisory Board and recognizes the team that earned the top overall design score. The winning team is able to: demonstrate that their design goals solve the chosen problem; justify their design selection; justify quantitative specifications; and produce clear drawings or diagrams. This group also earns placement on the BIOE Advisory Board Award for Translational Design trophy, which resides in A. James Clark Hall.
The MPower Award recognizes the team that demonstrated exemplary collaboration with the University of Maryland, Baltimore. This award is sponsored by representatives of the University of Maryland MPowering the State Strategic Partnership.
The Fischell Department of Bioengineering thanks its panel of Capstone judges, which this year featured members of the BIOE Advisory Board and members of our esteemed faculty.
The Fischell Department of Bioengineering receives support for its Capstone Design competition from the Fischell Family, the University of Maryland MPowering the State Strategic Partnership, and Expo event sponsor Whiting-Turner (WT). Additionally, Capstone students receive mentorship support from industry representatives and/or clinicians, including investigators from the University of Maryland School of Medicine, Children's National Health Center, the U.S. Food and Drug Administration, the UMD Robert E. Fischell Institute for Biomedical Devices.
Team 1: A Portable, Affordable Cardiopulmonary Exercise Device
Elizabeth Barski, Caroline Kelly, Abigail Miller, Anthony Qin, Olivia Stevens
AWARD FOR TRANSLATIONAL DESIGN
The COVID-19 pandemic heightened interest in telehealth and personal fitness. We designed a device to take advantage of these growing markets by providing a portable cardiopulmonary exercise test (CPET) for use in both the telemedicine and athletic world. Rather than replace medical-grade CPETs, this device will bring cardiopulmonary health tracking outside the lab, for more casual and convenient use. For telemedicine patients and athletes, the device will identify significant changes in cardiopulmonary health over time, reducing the need to visit a clinical lab or high-performance athletic facility. For patients with cardiopulmonary concerns, this device could be used at home under the guidance of a healthcare provider who can use the results to monitor patient health progression. For athletes–professional and now with our device, everyday enthusiasts–the device can monitor fitness, informing users of their aerobic capacity and allowing athletes to better tailor their workouts for maximum performance.
The device was constructed from a 3D printed case which holds an oxygen sensor, carbon dioxide sensor, arduino, and a homemade flowmeter with a differential pressure sensor. The miniaturized CPET can indicate basic cardiopulmonary health metrics on a Matlab application by measuring O2, CO2, and breath volume. Our device meets our technical specifications, including cost, with the prototype costing under $250 dollars, and size, being easily handheld and weighing 11.22 oz. Importantly, the device can also increase equality in research and clinical trials regarding cardiopulmonary health by reaching more broad populations and settings. As with any device that collects personal health information, the privacy of user data is of the utmost importance. Our device has the potential to bring the power of an advanced medical test into a hand-held apparatus available at home or in the gym for patients and athletes alike.
Team 2: Updated Gastrojejunostomy Tube - Limiting Tube Migration Patterns
Mark Boegner, Nikka Givpoor, Alison Grafton, Adriana-Isabela Melendez-Munoz, Kate Tanchanco
Advisors: Dr. Gregg Duncan, Dr. Diana Jo
Feeding tubes are needed by many children to deliver nutrients when there are issues in the digestive tract. They are used to bypass the mouth and esophagus and lead directly into the stomach or intestines. This specific project focuses on the gastrojejunostomy tube (GJ tube), which is placed into the patient’s stomach and small intestines. The tube has two main portions, the “G” portion, which remains in the stomach, and the “J” portion, that goes into the jejunum and is used to deliver food and nutrients to the patient. Proper function of this tube is crucial in ensuring the child gets the necessary nutrients. A common problem with GJ tubes is known as a “tube flip” where the tube migrates back up the digestive tract causing many adverse effects. To address this problem, a novel design utilizing a mucoadhesive layer underneath a biodegradable layer applied to the distal end of the GJ tube will be used. The biodegradable layer, a cellulose hydrogel, allows for easy placement of the tube. Cellulose was chosen due to its rapid degradation and biocompatibility. The mucoadhesive layer, a chitosan hydrogel, would then be revealed upon the cellulose degradation; chitosan was chosen due to its biocompatibility and adhesive properties, specifically, its ability to adhere to the intestines for an extended period of time in order to hold the tube in place without causing adverse effects to the intestinal wall. This design would limit the migration pattern of the GJ tube, thus relieving the adverse effects that come with it while maintaining proper functionality of the tube.
Team 3: Single-Step Tracheostomy Device
Liam Carmody, Corinne Martin, John Ritz, Daniela Tran, Sahar Zaidi
A tracheostomy is a medical intervention that restores lung airflow by inserting a tube in the trachea to bypass an upper airway obstruction. The standard-of-care procedure involves puncturing the trachea and using a series of progressively larger dilators to expand the opening and insert a tracheostomy tube. This process is inefficient for the physician, and the insertion and removal of multiple dilators increases the patient’s risk of tissue damage, oxygen deprivation, and infection. This project aims to produce a tracheostomy device that will allow the dilation and tube insertion to be performed in a single step, decreasing the complexity and risk of the procedure. To achieve this, we developed a device for use with the guidewire and tracheostomy tube used in the conventional procedure. The final prototype features a hinged dilator tip that is inserted into the tracheal puncture and expanded using an indirect screw mechanism. As the user turns the screw, a plunger advances linearly through the device, pressing the flanges of the tip outward, allowing a tracheostomy tube to be installed in the opening. Testing on ex vivo porcine trachea samples validated the efficacy of this mechanism and design, facilitating a shorter procedure duration and streamlined workflow. The impact of this is twofold: increased efficiency for hospitals and physicians, and improved outcomes for the patient.
Team 4: Virtual Reality Endoscopy Controller for Oculus Quest 2
Andrew Cleck, Trent Crumback, Reshma Ganesh, Ajeet Goraya, Alexander Long
This project addresses the challenge of improving training methods for endoscopy procedures, a minimally invasive surgical technique. Traditional approaches, such as apprenticeship and simulation-based training, have limitations; Apprenticeship-based training can lead to more error in live patients, while simulation-based training, a supplemental method of training, often lacks realism. Our team is developing a novel endoscope controller prototype for the Oculus Quest 2 Virtual Reality system. This prototype aims to provide a more realistic and safer training experience for doctors by replicating the feel and functionality of a real endoscope. The final prototype has similar housing in terms of size (device length: 9.5 in, handle length: 3.1in) and weight (2 lbs) to the endoscope. The functionality of the buttons and joystick is integrated to reflect the directionality and motion of the simulation software in the Oculus. By providing a more realistic, accessible VR training experience, our controller has the potential to reduce errors during real-world procedures.
Team 5: Optimizing Erythromer Testing Methods
Daniel Coile, Sophia Damico, Hannah Lee, Abhishek Malhotra, Fiona Sheridan
Advisor: Dr. Alisa Clyne and Dr. Allan Doctor
The US has recently experienced a significant decline in blood donations, leading to a blood shortage crisis. Current solutions include hemoglobin-based oxygen carriers (HBOCs) and perfluoro-carbon emulsions to create blood alternatives. While HBOCs may be the most promising solution, their interference with nitric oxide (NO) causes vasoconstriction and restricts blood flow. Erythromer (EM), a novel freeze-dried blood substitute composed of nanoparticle-wrapped hemoglobin, functions as an oxygen transporter. EM has a lipid shell that reduces NO scavenging; however, the EM design must still be modified to further reduce of NO interference. PEGylation of EM could reduce NO scavenging by moving the EM particles away from the vascular wall, where most NO is found. The goal of this project is to design research methods that quantify how PEGylation of EM affects viscosity and particle localization. We tested varied PEG sizes (2000 and 5000 g/mol) and different surface saturation percentages of PEG (0.3%, 3%, 5%). We found that the concentric cup double-gap method works better than cone and plate rheometry due to reduced evaporation and increased accuracy of measuring lower-viscosity fluids such as blood. We also found spinning disk confocal microscopy (SDCM) was a more effective method to quantify the inertial flow behavior of EM solutions in a resistance arteriole model compared to laser scanning confocal microscopy because it allowed faster image acquisition. Optimizing the methodologies for EM testing is important to enable future EM testing improvements, which in turn, make available an affordable and effective blood substitute that can be provided to those in critical need of blood.
Team 6: NEC-Detect: Point of Care Device using Colorimetric Assay for Necrotizing Enterocolitis Detection in Preterm Infants
Deborah Asfaw, Rony Garcia-Vivas, Zoe Sokol, Katherine Tom, Eitan Traum
Advisors: Clinical Mentor, Dr. Rose Viscardi / Faculty Mentors, Dr. William Bentley and Dr. Sara Molinari
Necrotizing Enterocolitis (NEC) is a life-threatening gastrointestinal disease that affects preterm infants (< 37 weeks). If not diagnosed early, it can lead to severe health complications and potentially death. Though NEC only affects 7-10% of preterm infants, the mortality rate for this disease ranges from 30-50%. The rate of disease progression can lead to mortality within a week of diagnosis in most cases. In severe cases, disease progression can lead to death within 24-48 hours of first symptoms. Previous research has concluded that formic acid, a short-chain fatty acid, is found at elevated levels in newborns who may be developing NEC. A 2023 BIOE Capstone Team developed a colorimetric assay to allow for easier screening of NEC in preterm infants through the detection of formic acid. Although this new assay shows promising results, NEC can still be costly and difficult to diagnose, as there are no at-home or bedside kits readily available to quickly determine results without proper laboratory equipment. NEC-Detect aims to provide a point-of-care device kit that rapidly and effectively detects NEC in NICU settings. The kit includes a small motorized centrifuge, capable of producing 12,000 Gs of force, Potassium Permanganate and PBS as assay reagents, and several novel tube caps to allow for sample collection, filtration, and detection. NEC-Detect will allow early detection and treatment of NEC while avoiding harm through accurate diagnosis and appropriate use of medical intervention. The kit design prioritizes ease of use by healthcare professionals with varying levels of training, ensuring equitable access and usability across different healthcare settings.
Team 7: Delivery of a Biodegradable Hydrogel to Improve Hemostasis After Intracerebral Hematoma Evacuation
Naomi Butler, Ruby Delgadillo Guerrero, Autumn Hengen, Joseph Kutza, Christus Quidlat
Advisors: Dr. Huang Chiao Huang; Dr. Riccardo Serra
Intracerebral hematomas (ICH) is a condition in which a blood mass or hematoma develops in the brain parenchyma. ICHs are associated with high morbidity and mortality rates. Approximately 40% of patients die within the first month, and only a small percentage (12 - 40%) receive long-term independence. Following ICH evacuation, postoperative rebleeding (PRB) is a common issue that contributes to higher mortality rates. Achieving homeostasis with this type of procedure is challenging; even with strategies like hemostatic injectables, there are still obstacles like capillary bleeding. In this project, we aim to create a biodegradable, injectable hydrogel that exerts pressure to prevent rebleeding. This hydrogel is fabricated from FDA-approved biomaterials, including poly(lactic-co-glycolic acid) and polyethylene glycol. At room temperature, the hydrogel is a liquid that allows easy administration into the patient via a syringe. At average brain temperature (38.5℃), the hydrogel solidifies into its active form and degrades as it interacts with native cerebrospinal fluid steadily. Furthermore, we aim to create a prototype system that simulates the hydrogel delivery in an ICH patient. This system consists of a model brain composed of agar, containing tubing through which blood can flow at a specified rate. Within the brain, there is also a cavity that recapitulates the cavity seen in ICH evacuation, where our hydrogel can be dispensed via a syringe for site management of the ICH, restoring healthy blood flow. Our system effectively simulates the methods for hydrogel delivery and resulting change in blood flow to prove therapeutic success of the intervention. This will provide an easier operation for doctors to treat ICH patients with fewer complications. For this to be accomplished, a series of animal tests will be done to assess the hemostatic efficacy, biocompatibility, and degradation of the animal models induced with ICH. It will move on to extensive human clinical testing, where consent will be obtained from patients who are at high risk of ICH rebleeding or getting consent from health care proxies about using this design. It will benefit the ICH patients and the doctors by providing a less invasive and less complicated solution to their rebleeding issues with their disease. This can be further improved by drug loading the hydrogel, application to other injuries, and developing effective storage mechanisms for the accessibility of low-income countries (LICs).
Team 8: Telemedicine Headphones for Pediatric Ear Health Assessment
Ariana Capati, Xavier Garcia-Collazo, Adebowale Hassan, Thien Dinh Lam, Maya Wheeler
Advisors: Dr. Kyung Koh, Children's National Hospital: Dr. Christopher Gable and Dr. Kevin Cleary
The current standard of care for diagnosing Otitis Media requires the use of expensive Otoacoustic Emission (OAE) equipment and frequent visits to healthcare providers. The costs of frequent visits puts a strain on healthcare systems, while the expensive equipment is inaccessible in low and middle income countries, leading to poor health outcomes. Our team’s solution is to develop a low-cost telehealth OAE detection device that can function in low resource areas and at-home settings. Our project is organized as follows: begin by building off of previously developed telemedicine earpods from an open source University of Washington design capable of OAE detection, test and update previous designs based on our pediatric specific design specifications, create a user-friendly telehealth platform for data collection and referral, and finally design a potential clinical framework in collaboration with Children’s National Hospital. Significant milestones achieved during prototyping include the finalization of a 3D printed physical prototype that can house necessary design hardware, development of a mobile application for comprehensive data storage and retrieval, and a framework for future testing at Children’s National Hospital. This device has the potential for numerous impactful outcomes, including more accessible detection of Otitis Media in pediatric patients, enhanced convenience for caregivers with a lower burden on healthcare settings, and promotion of early detection leading to enhanced antibiotic stewardship while mitigating the long term the effects unaddressed ear conditions.
Team 9: Accessible Ventilation Coach for Opioid Overdose Bystanders
Ashley Armitage, Adam Bizri, Colton Houldsworth, Ashani Ross, Kelly Yeung
Advisors: Dr. Jason Rose and Dr. Ian White
DEAN'S AWARD
With over 110,000 deaths in 2023, the rising opioid overdose epidemic in the United States has prompted an urgent need for accessible and cost-effective solutions to save lives outside of hospital settings. The number one cause of death from opioids is respiratory failure, and thus the best immediate treatment is to support respirations. This is performed by EMS using a Bag Valve Mask (BVM) when they arrive; however their typical response time ranges from 7 to 14 minutes. Although bystanders could save a person’s life by supporting respirations while awaiting EMS, safe use requires training. This project aims to develop an innovative adjunctive device to the widely available BVM that will empower families and non-EMTs to provide timely rescue breaths with proper volume and cadence. The device provides visual guide LEDs for the proper rate and depth of compressions, along with feedback LEDs synchronized with the user’s performance. An audio system is also included to provide coaching and feedback during device misuse. A pilot test involving the 6 designers showed an increase in user efficacy with improvements in breaths per minute and volume output when measured with a Michigan Test Lung. This solution holds promise in empowering untrained bystanders to deliver successful rescue breaths using a BVM, potentially revolutionizing the landscape of opioid overdose management and reducing mortality rates in affected communities.
Team 10: Novel Ventricular Catheter for Drainage of Cerebrospinal Fluid with Optimized Diameter and Anti-Clotting Specifications
Anjola Akintoba, Lauren Gabranski, Lauren Gomes, Diego Pantelis, Amanda Vecchio
Advisors: Dr. Erika Moore & Dr. Riccardo Serra
MPOWER AWARD
Ventricular catheters are currently a key piece of medical equipment being used to treat both chronic and acute cases of hydrocephalus and hemorrhages. However, the standard ventricular catheters that are available in hospitals rely entirely on drainage holes along the side portions of the catheter. This current model functions effectively for chronic forms of hydrocephalus, where the primary goal is to drain cerebrospinal fluid, however, issues often present themselves when this catheter is used in acute cases where blood clots frequently occlude the peripheral holes. Thus, the development of a novel ventricular catheter with a removable distal tip via a metallic stylet would allow for an additional fluid drainage site and a reduction in the need for such catheters to be replaced due to occlusion. The additional drainage route at the distal end of the catheter will be placed in the ventricle of the brain, minimizing the risk of damage to brain tissue in situations where the catheter needs to undergo a flushing procedure to dislodge blockages. The development and implementation of this device would be beneficial to physicians by reducing the number of emergency drain replacements that need to be performed, as well as improving overall patient outcomes by minimizing any tissue damage or infection that ultimately could result during a catheter replacement. However, in the testing and implementation of this device, it is vital that a wide variety of patient populations are used in clinical trials to ensure it provides universal favorable outcomes. Ultimately, it would also be important to consider the ethical implications of producing this product using materials and manufacturing methods that are minimally expensive to ensure that this product is available to patients and clinical settings regardless of financial factors.
Team 11: A Modified Syringe Design to Simplify the Preparation of Weight-Based Pediatric Medication
Heya Albiel, Sakshi Narula, Mariam Rahman, Matthew Walls, Heleena Zenna
FIRST PALCE
Medication dosage errors, especially in high-stress environments like hospital emergency rooms, pose a substantial risk to patient safety, particularly in pediatric care where dosages are weight-dependent. Current manual processes, involving weight assessment, tedious calculations, and medication preparation, are error-prone, potentially endangering patients' lives. To address this, we propose a cost-effective, user-friendly syringe-like device, specific to each drug and concentration. This device simplifies the workflow by allowing healthcare providers to immediately draw up the required dose knowing the patient’s weight. The design features a dose adjustment dial that can freely move up and down the syringe plunger and can be locked into place at the plunger ridges marking specific weights. The inclusion of the dose adjustment dial and other syringe modifications decreases time to draw medication, reducing time to administer medication in emergencies by over 40%. By streamlining this critical process, our innovation improves patient outcomes for pediatric patients, reduces risk of error for pediatric clinicians, and overall reduces liability and risk for hospital administration.
Team 12: Semi-Automatic Positioning Device for Magnetic Resonance Neuroimaging System
Avneet Bahra, Eli Fisher, Ryon Sarkarzadeh, Donaysia Torbit, Heather Wheeler
Advisors: Clinical Mentor: Dr. Konstantine Cherkas / Faculty Mentor: Dr. Giuliano Scarcelli
Small Animal Magnetic Resonance Imaging (SA-MRI) is used for preclinical and molecular MRI for small animal in-vivo imaging. SA-MRI combines functional MRI and tractography tensor imaging. Among the challenges of automating fMRI and STI processes is data acquisition as a function of subject positioning. Mismatch in isocentric positioning and inconsistency in subject loading can lead to spatial discrepancies and signal variability. The readjustment process is time-consuming and can lead to inaccuracies in imaging due to manual positioning. A semi-automatic apparatus tailored for aligning subjects within the MRI system proves to be effective in minimizing spatial discrepancies between subject and reference images along with dependence on registration softwares that align the images virtually. The redesigned cradle implements a head holder fashioned along a pair of rods that allow for sliding actuation, in the x-direction, by way of a stepper motor attached to a worm and pinion gear. The back of the cradle is supported by three rods and two screws attached to stepper motors, allowing for the rotation of the screws to move into/out of the machine, z-direction. These changes ensure minimal pain and discomfort for the small animal by using micrometric neck movement. Implementation of the new device will have a positive impact on reducing required anesthesia time and technician fatigue along with the need for manual manipulation of the scanned images.
Team 13: Transparent Clips for Surgical Treatment of Intracranial Aneurysms
Ana Boyd, Malachi Green, Hannah Moskios, Ashley Nguyen, Philip-Diamond Phillips
Advisors: Dr. Jacob Cherian and Dr. Kimberly Stroka
SECOND PLACE
An aneurysm is a weak or thin spot on an artery in the brain that balloons or bulges out and fills with blood. This can lead to pressure on the nerves or brain tissue, rupture, hemorrhagic stroke, brain damage, coma, or death. Each year in the United States, 6.7 million people suffer from intracranial aneurysms. In 30,000 of these patients, the aneurysm eventually ruptures and causes bleeding in the brain. The current standard of care for treating aneurysms is microvascular clipping with titanium clips. The clips are surgically placed around the neck of the aneurysm to inhibit blood flow. There are several limitations regarding this treatment method. Surgeons often have difficulty placing clips accurately, as the titanium material is opaque and therefore obstructs the view of the surgical site. This can lead to potential poor placement of the clips and increase the risk of postoperative complications such as aneurysm recurrence, aneurysm rupture, and vessel occlusion with consequent stroke. The titanium clips also show up as artifacts on MRI and CT angiograms when examining the patient’s brain post-operation. This makes it difficult for the doctor to see if the inhibition of blood flow to the aneurysm was successful. To address these issues, our team has developed a transparent aneurysm clip with similar closing force and geometry as the current standard of care clips. Our clips have high optical clarity, allowing over 99% of light to pass through and enabling surgeons to resolve details as small as 44 microns. This allows for improved surgeon visibility, increasing the procedure's success and reducing the risk of complications. Furthermore, our clips minimize MRI or CT angiogram artifacts, improving the clarity of postoperative blood vessel imaging. Based on these findings, our clips have a significant impact that will benefit both patients and clinicians.
Team 14: Non-ferromagnetic IV medical pole for patient delivery during MRI procedure
Austin Carter, Bintou Koroma, Daniel Liu, Bhumi Patel
Advisors: Dr. Stanley Fricke & Dr. Beatrice Kondo
Non-ferromagnetic IV poles are indistinguishable from their ferromagnetic counterparts because they have a similar design and use the same universal clamping system. This leads to situations where non-MRI safe ferromagnetic components are attached to MRI-safe non-ferromagnetic IV poles and vice versa, which can result in deadly projectile incidents. This occurred in 2023 when an MRI safe infusion pump was placed on a non-MRI safe IV pole and the pole became projectile. There needs to be a clear difference between the two types of poles and their attachment pieces to prevent these incidents from occurring. Our solution is to create a tapered-shaped pole that will be unique from a ferromagnetic pole. Additionally, due to the pole shape, universal clamps, usually used on ferromagnetic poles, will not attach to the redesigned pole. The pole will have clear and permanent labeling so that as the pole gets cleaned, the label will not rub off or fall off. During this project process, we created and prototyped several components of our system before settling on our final design. We ensured our pole had material stability through loading simulations and weight bearing tests. Chemical stability was assessed via a series of cleaning tests using medical standard equipment. Shareholder satisfaction was gauged via a design survey which included relevant components of our design. Regarding ethical impact, the fact that our pole is non-metallic is an ethical benefit because metal is non-MRI safe. There are various ethical considerations concerning the pole’s use by medical personnel. For example, the pole’s height and weight should be taken into consideration to ensure that it isn’t too high to cause issues with cleaning or grabbing necessary tools and that it isn't too heavy to cause issues with maneuverability. The labels on the pole should also be taken into consideration to ensure that it is at an eye-friendly level to prevent issues with distinction.
Team 15: The AI Scribe (VitAI)
Ravidu Hevaganinge, Priya Jain, Matthew Sipper, Yaqi Zhao, Aditi Thangavelu
Advisors: Faculty Advisors: Dr. Yang Tao & Anjana Hevaganinge , Clinical Advisor: Dr. Kristen Johnson; Sponsor: Children's National Medical Center
"The AI Scribe" project addresses the prevalent challenge of documentation overload among healthcare professionals, a leading cause of dissatisfaction and burnout. Conventional manual approaches to clinical note-taking are both resource-intensive and prone to errors. To alleviate this documentation burden, our product introduces an innovative solution integrating Whisper AI's speech-to-text capabilities and the BART (Bidirectional Auto-Regressive Transformer) model to automate the generation of History of Present Illness (HPI) from audio recordings of clinician-patient interactions. The process begins with real-time conversation capture, followed by automatic speech recognition models (ASR). Subsequently, employing advanced Natural Language Processing (NLP) techniques, we extract vital details such as symptoms and chief complaints, resulting in concise and clinically relevant HPI summaries. Using a wide variety of open-source dataset (aci-bench), our algorithm continuously refines model accuracy through iterative training. By combining these techniques, we were able to generate HPIs demonstrating high accuracy indicators through our performance metric “ROUGE,” which compares our generated summary to a gold standard written by a physician or medical scribe. Overall, "The AI Scribe" represents a transformative advancement that enhances documentation processes, reduces clinician burden, and fosters improvements in patient care quality.
Team 16: Pressure-Driven Blood Metering for Improved Sepsis Diagnosis
Abigail Bond, Nikki Nguyen, Aric Rozario, Sebastian Rutz, Meron Yonas
Advisors: Dr. John Fisher, Fischell Department Chair; Sponsor: Frans Feijen, Becton Dickinson
Sepsis is the intense bodily reaction that occurs to combat bacterial, fungal, or viral infections. This condition can lead to severe organ dysfunction and potential death. Timely diagnosis is crucial in managing sepsis, as the risk of death increases by up to 8% every hour when treatment is delayed. Diagnosing sepsis involves indicators such as white blood cell counts, creatinine levels, and lactic acid levels in blood tests, commonly done through the BD BACTEC™ blood culturing system. As volume is the most critical variable for the detection of microorganisms in blood cultures, the BACTEC™ culture bottles require a fill level between 8 - 10 mL to ensure accurate diagnosis. In partnership with BD, our project focuses on the development of a proof of concept for the efficacy of an automatic pressure-driven blood-metering device that accurately extracts 9 mL of patient blood within ±1 mL to reduce false sepsis diagnosis. This entails integrating a pressure sensor to monitor flow pressure, a processor for volume calculation, and a servo to halt blood flow upon reaching the desired fill level. Our prototyping results demonstrate the effectiveness of a pressure-driven volumetric device for blood metering. Additionally, our design allows for a cost-effective and simple solution, ensuring alignment with the BD BACTEC™ system's business model to enhance accessibility while maintaining quality standards. Thus, we strongly encourage BD to pursue further research to develop this into a market-ready product to improve patient outcomes and contribute to effective sepsis management in clinical settings.
Team 17: Autonomous Control Systems of VV-ECMO
Parker Desalvio, Maryam Iyer, Ritik Mehul Shah, Smriti Thomas, Jacob Wang
Advisors: Dr. Wu from the University of Maryland Medical Center
Venovenous Extracorporeal Membrane Oxygenation (VV ECMO) is a specialized technique for managing severe respiratory failure by diverting blood away from the lungs and using an external circuit to facilitate oxygenation and CO2 removal. Patients with any form of lung injury, fluid buildup in the lungs from transfusions for resuscitation, or infections benefit from VV ECMO. The incidence of acute lung injury (ALI) ranges from 3% to 33%, and mortality 12.8% to 33%. Blast lung injury (BLI) has an incidence ranging from 1.4% to 40% and mortality of 11% to 56%. Delayed treatment could increase mortality further, making easily accessible and effective treatment for lung damage critical to increasing patient survival rates. ECMO management requires doctors and medical staff to constantly monitor the machines as long as they are running which can be demanding especially at high patient volumes. In emergency situations, patients can experience extreme events such as: quick blood clotting, pump failures, and other complications. These situations often require immediate intervention to keep the patient safe. Our solution to this is to obtain autonomous monitoring and control of the ECMO system by implementing O2/CO2 sensors to assess patient vitals and respond with the appropriate decision to maintain a balance in gas flows and ideal patient conditions. Humans are more prone to error compared to automated devices, so our system could offer more precise, real-time adjustments, which improves patient outcomes and makes this life-saving treatment more accessible to a wider patient population. Automation reduces the workload on healthcare professionals and can provide them with detailed data analysis to support more informed decision making regarding treatments. Unfortunately the dependence on technology raises concerns about system failures, software errors, or inappropriate patient management decisions. An over-reliance on autonomous systems could lead to a decline in manual skills and the judgment required to manage ECMO without technological assistance. The ideal use of our system would be to find a balance between manual and automated work to provide the best possible care for patients in need of the ECMO treatment.
Team 18: High-Flux Hemofiltration System for Toxin and Solute Removal
Cade Bergeron, Daiyaan Jiaad Kabir, Farshad Mashhadi, Colleen Simmerly, Zeyu Zhong
Advisors: Dr. Goldberg & Dr. Grazioli, Dr. King; Sponsor: UMSOM
THIRD PLACE
This project sought to design and execute the creation of an ECMO-compatible hemofiltration system that utilizes a twelve-hemofilter parallel arrangement made possible via the design and implementation of 3D printed components. By tuning the overall surface area and using the basis of a standard ECMO system, we intended to resolve the current limitations of the traditional system and surpass filtration rates of non-dialyzable toxins. Our team developed a system capable of stably supporting a range of flow rates upward of 5-6 L/min, alongside creating and implementing a blood-viscosity mimic that was run through the 12-filter hybrid system. The implications of this project regarding its potential clinical impact are notable and serve as a promise for an efficient solution towards modern medicine as a widely applicable modality to tackle the growing challenges of acute poisoning presentations. In the future, the ECMO-hemofiltration hybrid system could be utilized to remove various dialyzable and non-dialyzable toxins, such as metformin and flecainide acetate, beyond clinically relevant rates.
Team 19: Development of a Sterile and Automatic Biopsy Gun for Cell Retrieval
Lucas Frankle, Udit Gupta, Sehaj Hira, Neel Panchwagh, Luke Zhao
Biopsies, surgical procedures that retrieve a small portion of tissue, are often performed for cancer patients as part of a standard protocol for diagnosis and prognosis. This procedure can also be used as a source of cells for the development of patient-derived cell lines or autologous cell therapies. Current biopsy instruments were designed with the purpose of diagnosis; but with the advent of new downstream technologies, new instruments need to consider research and manufacturing applications of biopsy samples. The current instrument uses a spring-loaded needle to cut small sections of tumor tissue. This “tru-cut” method has been used for decades as the standard mechanism of action. The sample is stored in the tip until it is subsequently scraped off the needle. Surgeons repeat this procedure multiple times to acquire enough tissue. This process exposes the tissue to contamination and is operator-dependent. This project aims to construct a biopsy instrument that can standardize the acquisition process and allow for increased sample collection with a decreased procedure time. The designed instrument has a unique needle tip containing multiple scarves in its outer sheath, and a screw-like inner needle that allows for the collection of multiple samples simultaneously. The needle can be retracted into the device such that the sample is stored in a sterile chamber for later retrieval. The new instrument increases collected tissue mass compared to the current device and decreases procedure time, removing the need for multiple insertions of the device. This has the potential to remove operator-specific tendencies or error from the tumor biopsy process and allow for standardization in the acquisition process. This will reduce procedure time for patients, decrease pain and complications associated with the surgery, and boost the therapeutic manufacturing process in the hopes of curing disease.
Team 20: A Deep Learning Framework for Morphological Analysis of Electron Microscopy Images of the SARS-CoV-2 Virus
Leonardo Buitrago, Miguel Martinez, Severin Zitany Vihossi Mahuto
Advisors: Dr. Lan Ma, Dr. Frank Delaglio, Dr. Syed Saif Hasan; Sponsors: Institute of Bioscience & Biotechnology Research, University of Maryland School of Medicine
In collaboration with the Institute for Bioscience and Biotechnology Research, our project is centered on designing an advanced image processing system that utilizes a convolutional neural network, specifically a U-Net architecture, to analyze synthetic two-dimensional images of SARS-CoV-2 viruses. The primary objective is to accurately segment the virus body from the image background and pinpoint the distinctive spike proteins, which are crucial for understanding the virus’s infectious mechanisms. By extracting and quantifying detailed morphological features such as the viral body's radius and the number of spike proteins, the system aims to provide vital statistics that can inform virological studies. This proof-of-concept system not only shows promise in enhancing precision and speed of virological research but also lays the groundwork of identifying potential therapeutic targets.